Research Article | Published 15 January 2019
Yusuke Horii, Kunio Hirano, Hideomi Sato, Takashi Ito, Ryosuke Chiba, Satoshi Moriguchi, Hiroyuki Deguchi, Makoto Tomoyasu, Tatsuo Tanita, Tamotsu Sugai and Makoto Maemondo*
Division of Pulmonary Medicine, Allergy, and Rheumatology, Department of Internal Medicine, 19-1 Uchimaru,Morioka, Iwate 020-8505, Japan.
Department of Thoracic Surgery, 19-1 Uchimaru, Morioka, Iwate 020-8505, Japan.
Department of Pathology, Iwate Medical University School of Medicine,19-1 Uchimaru, Morioka, Iwate 020-8505, Japan.
An extracellular matrix non-structural secretory glycoprotein called secreted protein, acidic and rich in cysteine (SPARC) plays a significant role in promoting cancer cell activity and altering a tumor’s microenvironment. Studies of SPARC expression in lung cancer have been few compared to those of other organ malignancies. Consequently, we performed this study to elucidate the relationship between SPARC expression of a resected tumor and a post-operative prognosis.
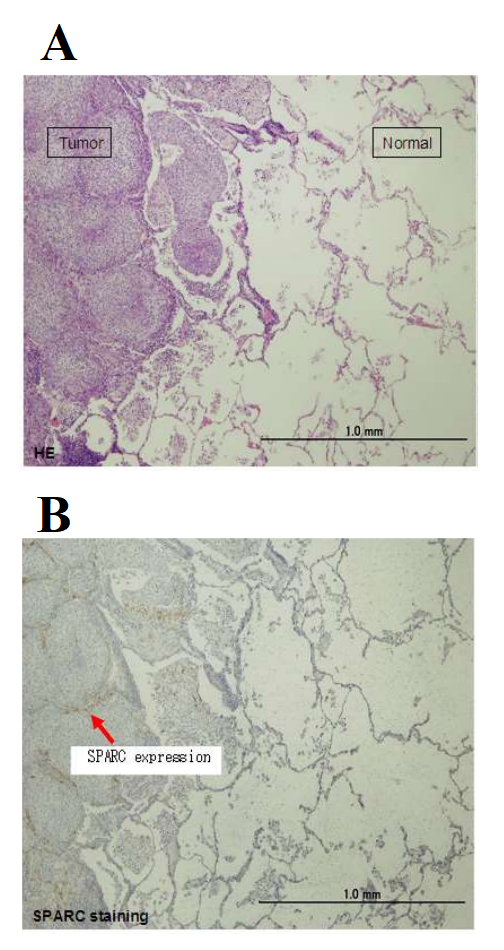
Methods: Postoperative patients with pulmonary squamous carcinoma or adenocarcinoma at Iwate Medical University Hospital from 2008 to 2012 were enrolled in this analysis. Operations enrolled patients underwent were restricted to lobectomy and lymph node dissection. SPARC expression in formalin-fixed paraffin-embedded sections obtained from specimens by surgical removal were evaluated by immunohistochemistry using a SPARC antibody. Data on patients’ characteristics and survival were collected from individual medical records.
Result: A total of 152 patients (87 adenocarcinoma and 65 squamous) were eligible for this analysis. Compared to cancer cells, the tumor stroma was predominately stained by an anti-SPARC antibody in immunohistochemical staining. The positive SPARC expression rate in squamous cell carcinoma and adenocarcinoma was 97% (63/65) and 62% (54/87), respectively. High SPARC expression of squamous cell carcinoma was related to poorer survival, but not of adenocarcinoma. This result was also observed in stage I squamous cell carcinoma. Conclusion: SPARC was higher expressed in squamous cell carcinoma than in adenocarcinoma. High expression of SPARC in squamous cell carcinoma was related to a poor prognosis. This suggests SPARC may be a prognostic marker of pulmonary squamous cell carcinoma.
Keywords:
SPARC, NSCLC, adenocarcinoma, squamous cell carcinoma, post-operation, immunohistochemistry, prognosis, stroma

MESFORD Publisher Inc is a premier global publisher of science, technology and medical resources. We offer unique, trusted content by expert authors, spreading knowledge and promoting discovery worldwide. We aim to broaden thinking and advance understanding in the sciences, providing researchers, academics, professionals, and students with the tools they need to share ideas and realize their potential